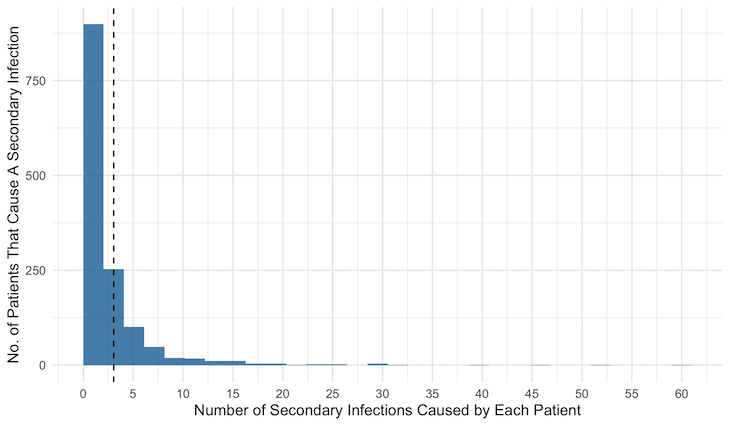
Of 17,008 Covid-19 patients who had tested positive and were contact-traced by July 7, only 1,381 or 8% had contacts who tested positive in the subsequent 14 days, by which time most infected individuals show COVID-19 symptoms, the government’s contact tracing data show. On average, each of these 1,381 patients infected three others while the remaining 15,627 (92%) caused no further infections, show data compiled by researchers at the Indian Statistical Institute (ISI), Bengaluru, from the state’s daily bulletins.
The government has disseminated contact tracing data for approximately 63.4% of the 26,815 cases confirmed in Karnataka by July 7, while the remaining cases were classified as “contact under tracing” in daily media bulletins.
Karnataka’s contact tracing exercise demonstrates the existence of the superspreading effect in India. “This is, overall, good news, since it implies that identifying super-spreaders is a powerful way of slowing down the progress of the pandemic and that most people will not transfer the infection to others,” said Gautam Menon, professor of physics and biology at Ashoka University in Haryana.
This can inform policies for relaxing some restrictions and maintaining those that help stem the ‘superspreading’, experts said. “Contact tracing still remains one of the most powerful tools that the epidemiologist has to prevent disease spread,” Menon said.
Source: Government of Karnataka, Department of Health and Family Welfare. Data compiled by Siva Athreya, Nitya Gadhiwala and Abhiti Mishra, COVID-19 India Timeline, the Indian Statistical Institute, Bengaluru.
Since the early days of the COVID-19 pandemic, experts have said that contact tracing is fundamental to a successful containment strategy, alongside widespread testing and quarantining. However, few Indian states have been successful in large-scale contact tracing.
India tests six known contacts per patient on average, as IndiaSpend reported on June 2, based on a study by the Indian Council of Medical Research (ICMR). Karnataka had the highest rate of contact tracing in the country, tracking 47.4 contacts per confirmed COVID-19 case in April, the study said.
Karnataka ranks high on measures of COVID-19 data transparency across Indian states, as per a new pre-print study by researchers at Stanford University in the USA. It is the only state that has regularly released contact tracing data in its daily bulletins, noting the contact status and origin of positive cases.
Researchers from ISI, Bengaluru, who have compiled these data caution that all data and analyses depend on different policies and rates of testing, population density, contact tracing, quarantine measures and the biological aspects of the epidemic. For instance, people in a particular cluster might have a greater chance of being tested as compared to a person in the general population, even though both might have contracted the disease, thus skewing the data on how the disease spread.
Study of source of COVID-19 infections suggest community spread
Central and state governments have repeatedly denied the presence of community spread, despite most cases now being locally transmitted, experts have noted. Community spread means that the virus is spreading “easily and sustainably” in the community, with the source of infection being unknown in large numbers of cases.
In Karnataka, cases associated with the influenza-like illness (ILI) and severe acute respiratory illness (SARI) categories, indicating that they were tested because of symptoms or contact with symptomatic patients, have been growing. Cases attributed to travel, which formed the majority of infections during the early months of the outbreak, have declined from 67% on June 1 to 12% by July 21. “This suggests that community transmission is present and growing,” said Menon.
ALSO READ: 'Rupture in digital world' as Trump orders ban on TikTok, WeChat in 45 days
“This is in line with the natural progression of the disease--it is initially imported from other areas and then local circulation starts to drive case growth,” said Giridhar Babu, professor and head of Life Course epidemiology at the Public Health Foundation of India.
Of the 55,826 cases confirmed in Karnataka between July 1 and July 21, 32,186 (57.6%) were of unknown origin while 11,931 (21.4%) and 2,366 (4.2%) were linked to ILI and SARI, respectively.
Overall, cases with an unknown source of infection, that is, where the “parent” case or contact was unknown, grew from 38.9% of cases by May 1 to 92.8% by July 21, data show. During this period, the number of confirmed cases grew 125 times, from 563 to 71,068 while the percentage of cases that were successfully contact-traced fell from 88.8% to 52%, calculations based on these data points show.
Source: Government of Karnataka, Department of Health and Family Welfare. Compiled and classified by Siva Athreya, Nitya Gadhiwala and Abhiti Mishra, COVID-19 India Timeline, Indian Statistical Institute, Bengaluru.
Note: ‘Unknown’ refers to cases classified as “Contact under tracing” in the Karnataka government’s daily bulletins. ‘Others’ had a known contact or reason for infection (e.g. healthcare workers, police personnel) but did not form large clusters.
Source: Government of Karnataka, Department of Health and Family Welfare. Data compiled by Siva Athreya, Nitya Gadhiwala and Abhiti Mishra, COVID-19 India Timeline, Indian Statistical Institute, Bengaluru.
Karnataka’s contact tracing exercise involves checking in with patients at multiple points to reduce errors and increase compliance with quarantine measures, as per the state government. Each patient’s contacts are traced at two points. First, patients are surveyed immediately upon testing positive and their details entered into the contact tracing application developed by the Karnataka government. Then, a field team follows up with the patient at their home, stamps their hand and puts up a home quarantine notice in front of their house.
After the contacts are identified, their details are verified by the field team who refer symptomatic contacts for immediate testing and prescribe home quarantine for asymptomatic contacts, who are tested within the next five-to-seven days.
In addition to contact tracing of infected individuals, in the early days of the pandemic, the government of Karnataka conducted a household survey through booth-level officers, covering 15 million households across the state. The survey identified people particularly vulnerable to the virus--the elderly, pregnant women and those with underlying health conditions. These people are now being regularly called and counseled through the Apthamitra teleconsultation helpline and their details have been shared with local health officers and ASHAs, who check on their health status and connect them with health resources for both COVID-19 and non-COVID ailments, the state government claims.
Over 10,000 government employees have been working as contact tracers in Karnataka, according to a note on contact tracing best practices shared by the central government’s Ministry of Health and Family Welfare on June 18.
Source: https://covid19.karnataka.gov.in/
‘Superspreading’ observed in other disease outbreaks
In Karnataka, 61 contact-traced patients were associated with more than 10 secondary infections each. Take for instance, patient 2,612, a 40-year-old male who travelled to Raichur district in Karnataka from Maharashtra. He was diagnosed on May 29 and was found to have spread the disease to 30 people. Similarly, as many as 18 contacts of patient 8,515, a 30-year-old woman who was tested in Ramnagar on June 20 after presenting ILI symptoms, also tested positive.
ALSO READ: Scientists decode how virus-carrying droplets disperse via breathing
The size of clusters caused by one individual expands further upon accounting for second- and third-order contacts. An analysis by Covid19India, a volunteer-run platform that has been compiling COVID-19 related data from across India, identified a cluster consisting of 242 people in the district of Bellary. Patient 4,350, a 52-year-old man diagnosed on June 5, infected over 50 other individuals. Many of these people had further contacts who tested positive, rapidly increasing the size of the cluster.
Source: Government of Karnataka, Department of Health and Family Welfare. Compiled and analysed by covid19india
This “superspreading” phenomenon, where a small number of people drive the majority of virus spread, is similar to patterns observed in other COVID-19 affected regions and other disease outbreaks, including those of the Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS).
In 2003, the first patient of SARS in Hong Kong infected nearly 125 others. In 2015, the first patient infected with MERS coronavirus (MERS-CoV) in South Korea caused 29 secondary infections, two of which further led to 106 of the 166 cases at the time.
The first 30 COVID-19 cases in South Korea, diagnosed over four weeks, did not cause many secondary infections. However, the 31st patient had over 1,160 contacts--fuelling the growth of the Daegu cluster, which accounted for 60% of all cases in South Korea in March. In May, a nightclub visitor in Seoul caused a resurgence of cases. Similar reports of a handful of individual infections leading to large clusters have emerged in the state of Punjab as well as in New York and meat packing plants across the US, and countries such as Jordan and Ghana.
“The spread of the virus is governed by the Pareto Principle”, according to which 80% of effects are driven by 20% of causes in many events, said Babu. “Only 10-20% of infected people are responsible for the actual spread” of COVID-19, he said.
‘Superspreader events and not superspreader persons’
Preliminary research on COVID-19 suggests that superspreading is driven by environmental factors and individual behaviour.
The SARS-CoV-2 virus is transmitted through direct contact, droplets in the air and contaminated surfaces. This makes closed spaces particularly susceptible to accelerating the spread of the virus. Japanese researchers identified COVID-19 case clusters in health facilities, restaurants, bars and gyms, indicating that the “three C’s”--closed, crowded and close-contact settings--fuelled superspreading.
It is also possible that some infected individuals “shed” more of the virus, increasing the viral load they expel into the environment that makes them more infectious, though research on this front remains tentative. Babu noted that individual viral load plays only a secondary role to context and surroundings in fuelling the spread of the virus. “I would not say there are superspreader persons but only that there are superspreader events,” he said.
Asymptomatic patients who do not know they are sick may put those around them at risk by failing to take adequate precautions or self-isolate, but the degree of their infectivity remains unknown. “We do not know yet whether asymptomatic patients can also act as superspreaders,” said Menon.
ALSO READ: Lupin launches Covid-19 drug Favipiravir in India at Rs 49 per tablet
Knowledge of superspreading patterns should inform policy
In Karnataka, during April and May, most cases were related to travel from other countries and domestic migration. After the relaxation of restrictions on inter-state mobility in the fourth phase of the lockdown starting May 18, the increase in new cases was driven by travellers from Maharashtra and their contacts. Seeing this cluster grow rapidly, the Karnataka state government enacted mandatory institutional quarantine for returnees.
To take preventative measures, it is important to understand the factors that make infected individuals potential superspreaders in the Indian context. “Correlating potential super-spreaders with their occupations is crucial,” said Menon. “It is very important to ensure that people in positions where they interact with many members of the public, e.g. vegetable vendors, healthcare workers and police personnel, are tested at regular intervals.”
Through contact tracing, the authorities can assign cases to various clusters, track the varying trends in growth and take policy steps accordingly. For instance, given the likelihood of superspreading in closed spaces, “any space that is closed where a large proportion of people are congregating for any reason should be avoided for the next several months”, Babu said, adding, “Kerala has banned all social gatherings till July 2021.”
Contact tracing mechanisms overburdened as cases increase
After weeks of slow growth, cases in Karnataka have increased over 20 times in the last two months--rising from 3,221 on June 1 to 15,242 on July 1, and from 67,420 on July 20 to 145,830 on August 5. Because of this increase, Bengaluru went back into a weeklong lockdown from July 14 to July 22.
With cases rapidly increasing, the contact status for many patients remains unknown as the government struggles to deal with the surge. Untested samples have piled up as Karnataka has rushed to expand testing capacity, even though the state government has instructed districts to ensure testing centres provide COVID-19 test results within 72 hours.
Tamil Nadu is expanding its contact tracing efforts after a large increase in cases associated with the Koyambedu Market in Chennai in May. The municipal corporation of Chennai has recruited 200 additional contact tracers to aid in more intensive tracing efforts in the city, The Hindu reported on July 23. The city has reported 104,027 COVID-19 cases, of which 11,859 were active by August 5.
As cases continue to rise, the Karnataka government assigned 1,246 employees to aid in contact tracing efforts, the Deccan Herald reported on July 7, 2020. The Bengaluru municipal corporation said they may only trace “primary contacts”, or immediate family members, instead of tracing all contacts who may have been in close proximity with the infected person or travelled with them, as was the earlier protocol, the Bangalore Mirror reported on July 1.
“Contact tracing is always useful but, given the increase in the number of cases and the lack of people trained in contact tracing, achieving extensive coverage will be more difficult in the future in states with large and growing numbers of cases,” said Menon.
ALSO READ: Uber rides take coronavirus hit but food-delivery business doubles
Kerala, which became the first state to acknowledge the presence of community transmission on July 17, is in the process of redeploying contact tracing staff towards curative operations, Livemint reported on July 21.
With limited contact tracing, “regular ILI surveys at greater frequencies such as once in two weeks, self-reporting for ILI, pharmacies reporting purchases of medicines for ILI etc. could help us continue to track the spread of the disease”, Babu said.
However, contact tracing should still form an important part of strategies in states with small numbers of cases. “States that are in the earlier stage of the epidemic, where most infections are still coming from travellers from outside, will benefit significantly from carrying out extensive contact tracing,” said Babu.
The “reproduction number” (R) of a disease is the average number of infections each patient may cause. The natural reproduction number (R0), the number of people infected in a completely susceptible population without a vaccine or physical distancing or use of masks, measures the natural infectivity of the virus. The effective R varies based on preventive measures, societal context and the level of immunity in the population.
The estimated R for COVID-19 in Karnataka is about 1.29 based on data from July 18-28, as per calculations by Sitabhra Sinha, a professor at the Institute of Mathematical Sciences in Chennai. However, not every infected person will cause further infections. The “dispersion factor” (k) measures the degree of homogeneity in how infected individuals spread the virus. A lower k would imply that a small proportion of infected individuals drive the spread while the majority of individuals cause few secondary infections. In a low k scenario, the disease is likely to spread in clusters fueled by superspreaders. A higher k indicates homogeneity in individuals’ infectivity, indicating that the virus will spread uniformly.
Preliminary estimates of COVID-19’s dispersion factor vary. A study of early outbreaks around the world placed COVID-19’s dispersion factor at 0.1, indicating that around 10% of infectious cases had caused 80% of secondary transmissions. Another study of 391 cases and 1,286 contacts in Shenzhen, China, published on April 27, 2020, estimated the dispersion factor to be 0.58, indicating 8.9% of cases had caused 80% of infections.
Analysing Karnataka’s contact tracing data until June 26, ISI researchers estimate that the dispersion factor varies from 0.06 in containment zone clusters to 0.21 and 0.18 in cases associated with the Tablighi Jamaat congregation in New Delhi in March and a pharmaceutical company in Nanjangud, Karnataka, respectively. These variations could be driven by a number of factors, such as the degree of case containment, which would affect an individual's mobility and ability to infect others, and extent of testing and tracing, which impacts the availability and quality of data on the clusters.
These estimates are similar to those for SARS and MERS, whose k has been 0.16 and 0.25, respectively. This indicates that 70% of SARS patients caused less than one secondary infection each, while 6% of the most infectious patients were associated with more than eight secondary infections.
(Bharadwaj, a recent graduate of Yale University, is an intern with IndiaSpend.)
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.
To read the full story, Subscribe Now at just Rs 249 a month
Already a subscriber? Log in
Subscribe To BS Premium
₹249
Renews automatically
₹1699₹1999
Opt for auto renewal and save Rs. 300 Renews automatically
₹1999
What you get on BS Premium?
-
Unlock 30+ premium stories daily hand-picked by our editors, across devices on browser and app.
-
Pick your favourite companies, get a daily email with all news updates on them.
Full access to our intuitive epaper - clip, save, share articles from any device; newspaper archives from 2006.
Preferential invites to Business Standard events.
Curated newsletters on markets, personal finance, policy & politics, start-ups, technology, and more.
Need More Information - write to us at assist@bsmail.in



)